By Dr. Ciprian Ionita, Research Assistant Professor of Biomedical Engineering and Neurosurgery in the School of Engineering and Applied Sciences and The Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo.
Personalization and customization have always been important goals in patient care. Even three years ago, physical modeling of a patient’s anatomy seemed out of reach. Today, Stratasys 3D Printing Solutions have made that level of personalization a reality.
The future of medicine is paved here, where my university collaborates with a private hospital via the Jacobs Institute (JI) – all housed in one building in Buffalo, New York. The 3D printed models we produce deliver patient-specific customization, enabling surgeons to build truly personalized treatment plans and device selection.
Current Surgical Limitations
There are several limiting factors for successful endovascular—meaning inside the blood vessels—image-guided intervention. These include medical imaging (CT scans, angiograms, and X-rays) and restricted movement within the arteries. For example, surgeons currently assess patients based on medical images rendered only in two dimensions, thus limiting understanding of patient-specific anatomy. Using 2D images as a guide, surgeons then remotely actuate the catheter tips using a push-pull or turn motion outside the body. These constraints mean added difficulty – especially for patients with complex, twisted arteries. Surgeons simply cannot visualize the full anatomy in the 2D model.
3D Printing: Empowering Surgical Planning
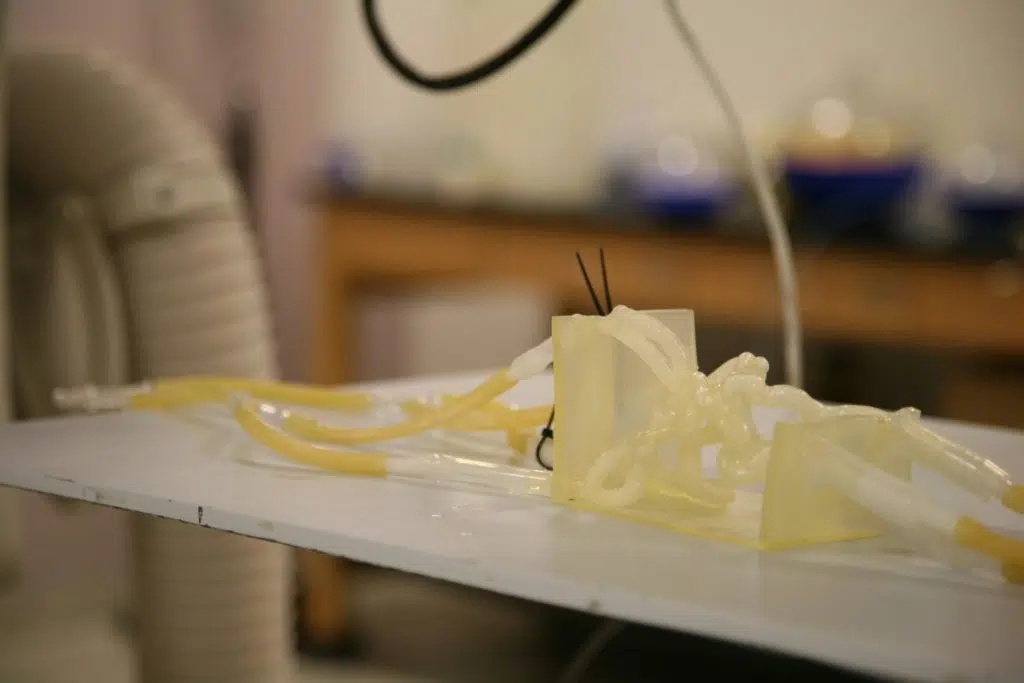
Dr. Adnan Siddiqui demonstrates deploying a medical device in a 3D printed model in a research laboratoryOne new approach is patient-specific “vascular phantoms” – or 3D printed models of brain vessels – alongside the medical imaging system. This “phantom” is perfect for physical measurements, treatment testing, physician training, and physiological simulations. By employing the Stratasys Objet Eden260V 3D Printer, our team works with phantoms to nearly the same resolution as medical imaging. Additionally, the flexible TangoPlus™ photopolymer material closely resembles human tissue, offering surgeons a life-like feel.
Our team first began 3D printing brain blood vessels in August of 2013. Since then, we’ve refined this workflow significantly – and are able to manufacture a patient-specific 3D vascular phantom within five hours. This means practicing complex surgeries – such as an aneurysm or stroke with abnormal vessel anatomy—before even walking into an operating room.
Dr. Adnan Siddiqui, Vice Chair and Professor of Neurosurgery at the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo, has successfully used the 3D printed phantoms: “Based on the Stratasys 3D printed models, we are able to pre-empt potential complications and devise a much more optimal means of treating an aneurysm.”
Beyond Surgical Benefits
Fluoroscopy image of 3D printed model of arteries that supply blood to the brain3D printing additionally offers a range of diverse applications in a clinical setting, including physician training and medical device testing. The JI regularly hosts training sessions for neuro and cardiac device companies – many of whom require models to teach and practice deployment of devices such as stents, clot retrievers, and balloons. These realistic models help sales representatives, R&D engineers and executives understand and feel how devices behave in life-like situations. This knowledge is crucial, especially for engineers working on improvements.
Modeling also drives new paradigms for teaching, entrepreneurship and innovation. The approach enables students and surgeons to practice on highly complex representations in a safe environment without using animals or cadavers. Further strengthening our commitment to vascular medical device innovation – realistic modeling is now mandatory when testing devices for safety and efficacy. Individuals with ideas for new or improved devices can easily deploy them in a faster, safer, and more cost-effective way via 3D printed blood vessels.
What the Future Holds: 3D Printing in Medicine
3D printed stroke model with embedded, simulated clot in middle cerebral arteryThe future of 3D printing will foster even greater personalization. Using patient-specific phantoms, 3D Endovascular Treatment Planning (ETP) now becomes an affordable pre-surgical necessity – the perfect fit for clinics employing 3D printers to speed the adoption of 3D ETP as a viable safety tool. The technology also addresses clinical challenges facing interventionalists in the angiography suites. That’s why we’re looking to further improve diagnostic and therapeutic efforts for the heart and vascular disorders in other organs.
At the same time, safety and patient care during surgery can be improved. Backed by 3D ETP, interventionalists now evaluate approaches for patients with difficult arterial anatomies – while surgeons leverage the technology to make more informed choices during device evaluation. Ultimately, 3D ETP cuts surgical time, reduces risks of adverse events, and lowers radiation exposure to the patient. From a commercial perspective, modeling techniques improve bench-top model testing for medical device manufacturing companies – therefore resulting in fewer device failures during animal and clinical trials. This creates a realistic forum to test device safety and efficacy.
As we continue to grow with Stratasys, this is just the tip of the iceberg. The future is truly unlimited for JI – driving better patient outcomes with forward-thinking surgeons backed by the power of advanced 3D printed modelling.
Click here to see how surgeons use a Stratasys 3D printed vascular model of a brain aneurysm to save the life of a mother of three.